Cramping
Cramping in the legs is a very common symptom of vein disease (also known as chronic venous insufficiency), which is the result of malfunctioning valves in the veins and poor circulation in the legs. When your veins are not pumping blood properly, rather than traveling in a smooth single direction, blood can flow backwards and pool in the veins, leading to cramps and “charley horses.”
How is leg cramping related to my veins?
Leg cramps are your body’s way of warning you that something has gone wrong within your veins. Functional, healthy veins do not experience pain, discomfort, swelling, cramping, itching, or other uncomfortable symptoms of vein disease. If you experience cramps in your legs unrelated to exercise (such as long hikes, frequent running, or squats), and that occur around visible varicose veins, the cramps are likely the result of vein disease. When vein disease progresses, leg circulation suffers, which can result in legs starting to cramp, feel heavy, and become painful.
What causes leg cramps?
Cramping in the legs, like any symptom of vein disease, can be caused by many factors both within and outside of our control. Hormonal imbalances, lifestyle choices, genetic predisposition, and frequent travel can result in varicose veins, and their symptoms will worsen over time if left untreated. The main culprit and common factor is poor circulation.
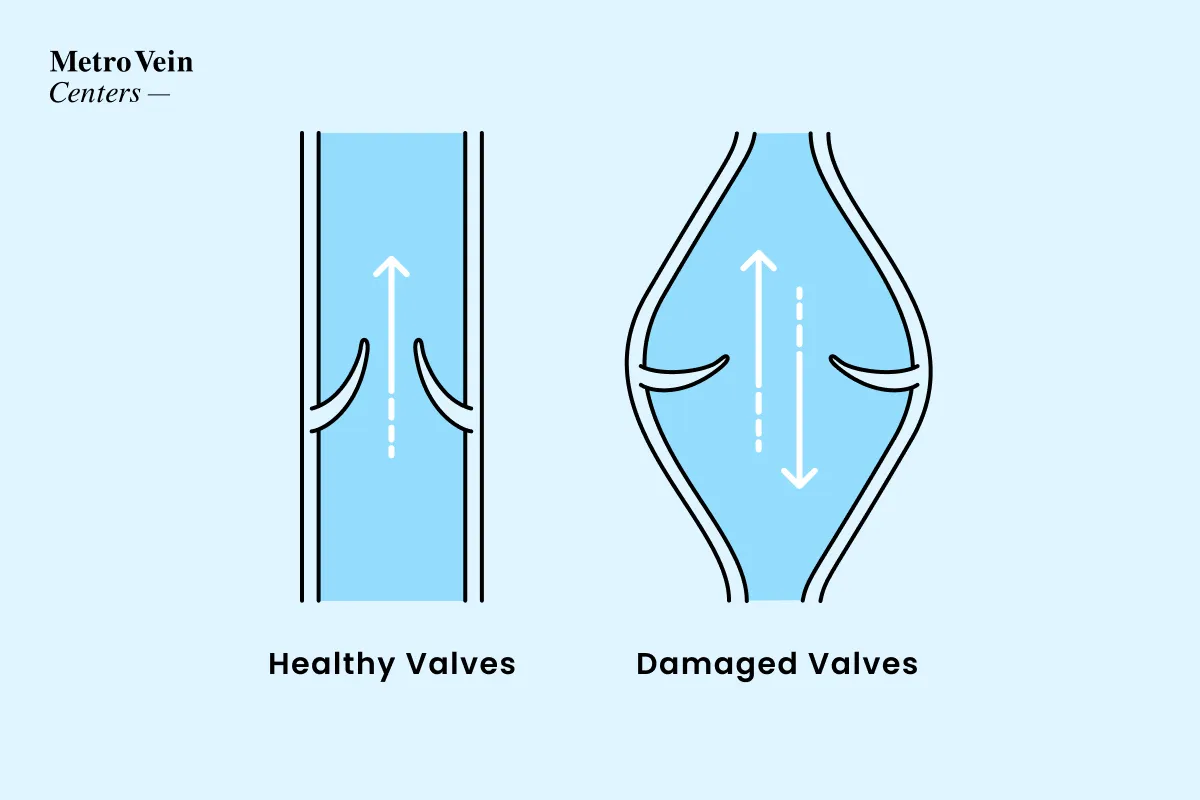
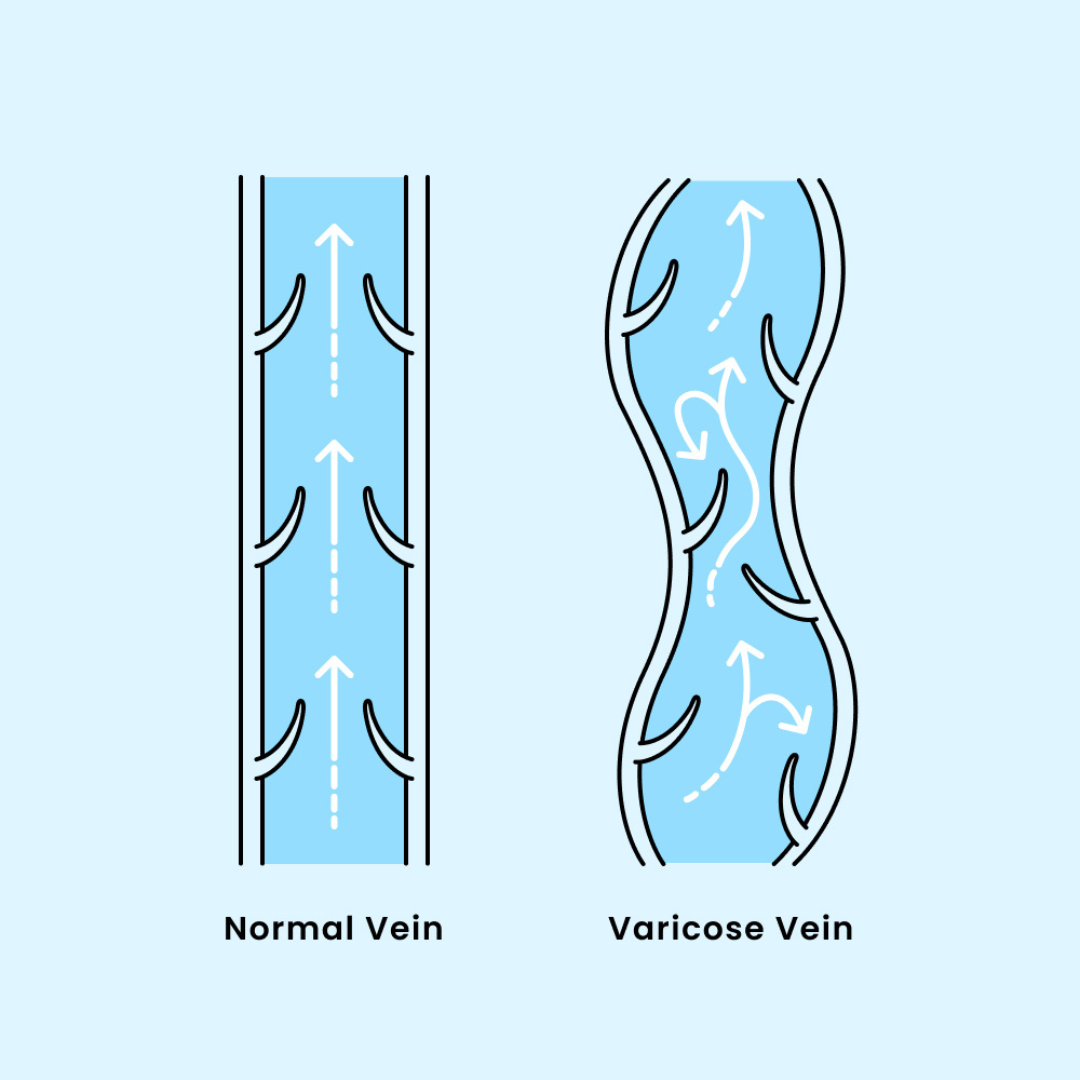
Blood is meant to flow in one direction around the body, and veins have protective valves that ensure this blood flow is maintained. When circulation suffers, as is common in the legs, these valves can become damaged and blood can start flowing in both directions and pool in the veins. This blood pooling begins to distort your veins, causing often-visible bulging, twisting, cord-like veins to protrude against the surface of your skin. As varicose veins (also known as varicosities) worsen, other symptoms such as aching, tingling, itching, cramping, and swelling may appear.
With cramping, it’s important to note that alcohol and caffeine are vasoconstrictors (substances that cause the veins to constrict, temporarily affecting circulation). So daily coffee consumption and frequent alcoholic drinks may worsen leg cramping, especially if a person isn’t drinking a lot of water. Neither coffee or alcohol are causes of vein disease, but they can affect the intensity of your symptoms.

What are the risk factors for cramping?
Varicose veins, and related symptoms like cramping, can result from genetic and/or lifestyle factors. Anyone, regardless of how active or inactive they are, can develop varicose veins, and they aren’t always visible to the naked eye. Symptoms such as aching, heaviness, swelling, and restless legs associated with vein disease can be caused by damaged veins under the surface.
Do you…
- Smoke?
- Travel frequently and/or for long periods by air?
- Lead a sedentary lifestyle?
- Have a family history of vein disease?
- Take hormonal birth control?
- Have diabetes?
- Drink alcohol often?
- Consume one or more cups of coffee daily?
Are you…
- A pregnant or postpartum woman?
- Over the age of 50?
- Diagnosed as overweight?
Anyone can develop varicose veins and vein disease due to hereditary factors, job stressors, and lifestyle. Though women are far more likely than men to have varicose veins, men are a significant percentage of patients. In fact, 2 out of 3 women and 1 out of 3 men will develop some form of vein disease during their lifetime. Factors such as standing on your feet all day, age, pregnancy, and increased weight are just a few reasons why certain people suffer from painful varicose veins. Cramping can be made worse by low fluid intake and/or overindulgence in alcoholic beverages. It also may be more noticeable for those who regularly drink caffeine*. Hydration is key in keeping your veins healthy—working with your circulation is key in symptom management.
*We’re not asking you to kick coffee—just make sure you’re drinking an equal or greater amount of water when you enjoy your daily cup of joe!

What can you do to treat and prevent cramping in the legs?
Cramping as a result of vein disease can be treated with a wide variety of FDA-approved and minimally invasive varicose vein treatments that we offer in our vein clinics. From radiofrequency ablation (RFA) to sclerotherapy and varithena, we’ve got you covered. Because it is a medical condition that causes symptoms, such as cramping legs that impact your daily life, vein treatment is covered by most insurance providers. We accept more than 200 insurance plans and are happy to discuss the details with your vein specialist, who will develop a custom treatment plan for your unique needs..
Unfortunately, preventing cramping legs without vein treatment is not always possible, as many factors such as genetics, familial history, sex/gender, and even weight are outside of our control. However, there are some lifestyle changes that can decrease your risk for developing varicosities and managing the cramping that results from vein disease. Quitting smoking, maintaining a healthy weight, eating a balanced diet, staying hydrated, and exercising regularly can improve circulation and lessen the chance of varicose vein development. Even light exercise has been proven to promote healthy blood flow. Your vein doctor may recommend a decrease in your caffeine and alcohol intake, or simply an increase in your water intake, to help decrease the severity of your cramps. Wearing compression socks and elevating the legs also improves circulation and can provide temporary relief from symptoms.
If you have noticed varicose veins on your legs or are concerned about varicose veins developing due to lifestyle choices and/or family history, the best course of action is to see a vein doctor. Vein disease is progressive; it’s best to get checked as soon as you notice symptoms or visible signs of varicosities. For more information on varicose veins, book a free evaluation at one of our convenient vein clinics. We can be reached at 866-629-9848 with any questions.
Cramping Myth Busting Q&A
Varicose veins (and other symptoms of chronic venous insufficiency) will worsen over time if left untreated. Because vein disease is progressive in nature, postponing treatment in the hopes that your visible veins or cramping will go away can end up doing further damage to your body. Varicose veins left untreated can lead to loss of mobility, blood clots, and even venous ulcers (in severe cases). Varicose veins, due to the permanent malfunction in their valves, cannot revert back to normal unless treated. Think of them like a broken bone: to prevent the bone from healing incorrectly, it needs to be set. For your circulation to return to a healthy state, blood must rerouted away from the diseased vein.
For those who work on their feet for long periods of time, it may be harder to determine whether their legs are cramping from strain or from complications of vein disease. One of the key factors to note is the frequency of your cramping: if your legs ache during downtime or time off from work, if the cramping is affecting your sleep, and if your cramps are worse after caffeine or alcohol, your cramps are likely related to vein disease. Cramps in the legs that are unrelated to exercise or exertion (jogging, long periods of standing) and injury are often also a sign of vein disease.
The only way to know for sure, though, is to consult a board-certified vein specialist. Vein doctors will evaluate your symptoms and use an ultrasound to evaluate the veins beneath the surface of your skin that may be causing your cramping.
Unfortunately, as with all symptoms of vein disease, the only solution is to treat the source. Varicose veins do not resolve without treatment, and the symptoms of varicose veins are no different. While better hydration has a wealth of health benefits (including improvement to circulation), if your legs are cramping as a result of vein disease, your cramps are likely to worsen over time if your varicose veins are left untreated. Because chronic venous insufficiency is a progressive disease, symptoms will continue to disrupt or inhibit your day-to-day until treatment fixes the underlying cause.
Drinking more water may offer a slight improvement in circulation, but if you’re experiencing chronic cramping in your legs, it’s best to seek professional medical assistance to permanently resolve the issue.
How do Vein Treatments Work?
Vein treatments work by closing off unhealthy veins, just in different ways! Once closed, blood flow naturally reroutes through neighboring healthy veins.


Cramping Treatments
- State-of-the-Art
- Ultrasound Guided
- Less Than 30 Minutes
- FDA-Approved
- Minimally Invasive
- Minimal Downtime
Let’s talk about you
What are your veins like?
Get a snapshot of your vein health in just a few clicks.