Phlebitis refers to inflammation of one or more veins, often caused by a blood clot known as thrombophlebitis. Veins in the legs must remain open and unobstructed to facilitate blood flow to the heart. Vein disorders can restrict this blood flow, primarily due to inflammation. When a vein becomes inflamed, this is referred to as phlebitis. Phlebitis can be superficial (near the surface) or deep.
Phlebitis usually occurs in the leg but can be present in other areas of the body as well. Symptoms can be observed in the affected area where the inflamed vein is located.
Read on to learn more about phlebitis, some common causes, risk factors, and treatments.
What is Phlebitis?
Phlebitis refers to the inflammation of a vein, often triggered by a blood clot or injury to the vein walls. This condition can affect veins close to the skin's surface (known as superficial phlebitis) or deeper veins, a more serious condition called deep vein thrombosis (DVT) when a clot is present.
Phlebitis Types
Superficial Phlebitis
This type affects veins near the skin's surface. It is the mildest form of inflammation and usually gets better without treatment. When a thrombus is the reason for inflammation, it is termed superficial thrombophlebitis.
Deep Phlebitis
Is a more serious form of inflammation that occurs in the deep veins when a blood clot forms known as deep vein thrombosis.
What Causes Thrombophlebitis?
Thrombophlebitis occurs when a blood clot forms inside a vein, most often caused by irritation in, or injury to, the inside of a blood vessel.
Risk Factors for Phlebitis
Although not direct causes, there are also certain risk factors that are associated with vascular health issues and a higher risk of developing phlebitis, including:
- Pregnancy: Increases in blood clotting proteins, slows blood flow, raising the risk of clots and varicose veins.
- Surgery: Superficial phlebitis can occur as a result of certain medical or surgical procedures.
- Obesity: Too much weight can add pressure on leg veins, impeding blood flow and increasing inflammation.
- Blood Disorders: Disorders like anemia and Sickle Cell can increase the risk of vein inflammation.
- Increased Risk of Blood Clotting: certain prescription medications, genetic clotting disorders, cancer, and connective tissue disorders can all increase the risk of blood clots and phlebitis.
- Smoking: Cigarette smoke increases the risk of plaque buildup in the vessels.,.
- Vein Disorders: Both varicose veins and chronic venous insufficiency can increase the risk of phlebitis.
- Immobility: Sitting or standing too long can add pressure on the veins, leading to inflammation.

What are the Signs and Symptoms of Phlebitis?
Phlebitis can affect veins in the arms or legs. Phlebitis often manifests with one or more of the following signs and symptoms:
Visible Signs
- Swelling in the affected area
- Visibly bulging veins
- Redness in the affected area
- Hardened veins
Physical Symptoms
- Pain or tenderness
- Skin that feels warm to the touch
- Leg heaviness
- Fever- if an infection causes phlebitis, you may also have a low-grade fever.
How is Phlebitis Diagnosed?
To diagnose phlebitis, your doctor may inquire about any symptoms or discomfort you've been experiencing, or any changes in the affected area. They will also perform a physical examination to check for signs of swelling, skin changes, or tenderness. Additionally, they may assess the pulse in your leg and foot.
After the physical exam, the doctor may order several blood tests to identify potential causes of vein inflammation, such as blood clotting disorders or other blood-related issues. Additionally, it is common to conduct imaging of the affected leg. They might request an ultrasound, CT scan, or to examine the entire vein and assess blood flow.
Superficial and Deep Phlebitis Treatment Options
Some cases of phlebitis can be managed at home, though advanced cases require medical intervention. Treatment options for superficial and deep phlebitis differ and may involve:
- Conservative Management: Conservative treatments are best for superficial phlebitis, though they can relieve the symptoms of deep phlebitis. They include heat therapy, compression socks, and leg elevation.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can manage mild pain and swelling. However, if you have a blood clot, you may receive blood thinners or anticoagulants to treat it.
In advanced cases of thrombophlebitis, you may require surgery. Current surgical interventions include:
- Inferior vena cava filter placement
- Venous thrombectomy
What are the Complications and Associated Risks of Phlebitis?
Complications of phlebitis include:
- Deep Vein Thrombosis (DVT): DVT is a blood clot that forms within a deep vein.
- Pulmonary Embolism: A pulmonary embolism occurs when a blood clot breaks away from a deep vein and lodges in the lungs. This is a life-threatening condition that requires emergency treatment.
- Chronic Venous Insufficiency (CVI): CVI occurs when veins are damaged, making it difficult for blood to flow to the heart.
Phlebitis Prevention Strategies
Even if you're at risk of developing phlebitis, lifestyle modifications can help manage or even prevent the condition.
They include:
- Regular exercise to improve blood flow in the leg veins.
- Losing excess weight to reduce pressure on the veins.
- Managing the conditions that lead to phlebitis.
- Following directions for managing intravenous lines.
How to Live Well with Phlebitis
It is possible to live well with phlebitis by following a healthy lifestyle that incorporates a balanced diet, regular exercise, and lifestyle adjustments.
A few tips you can follow today to improve your condition include:
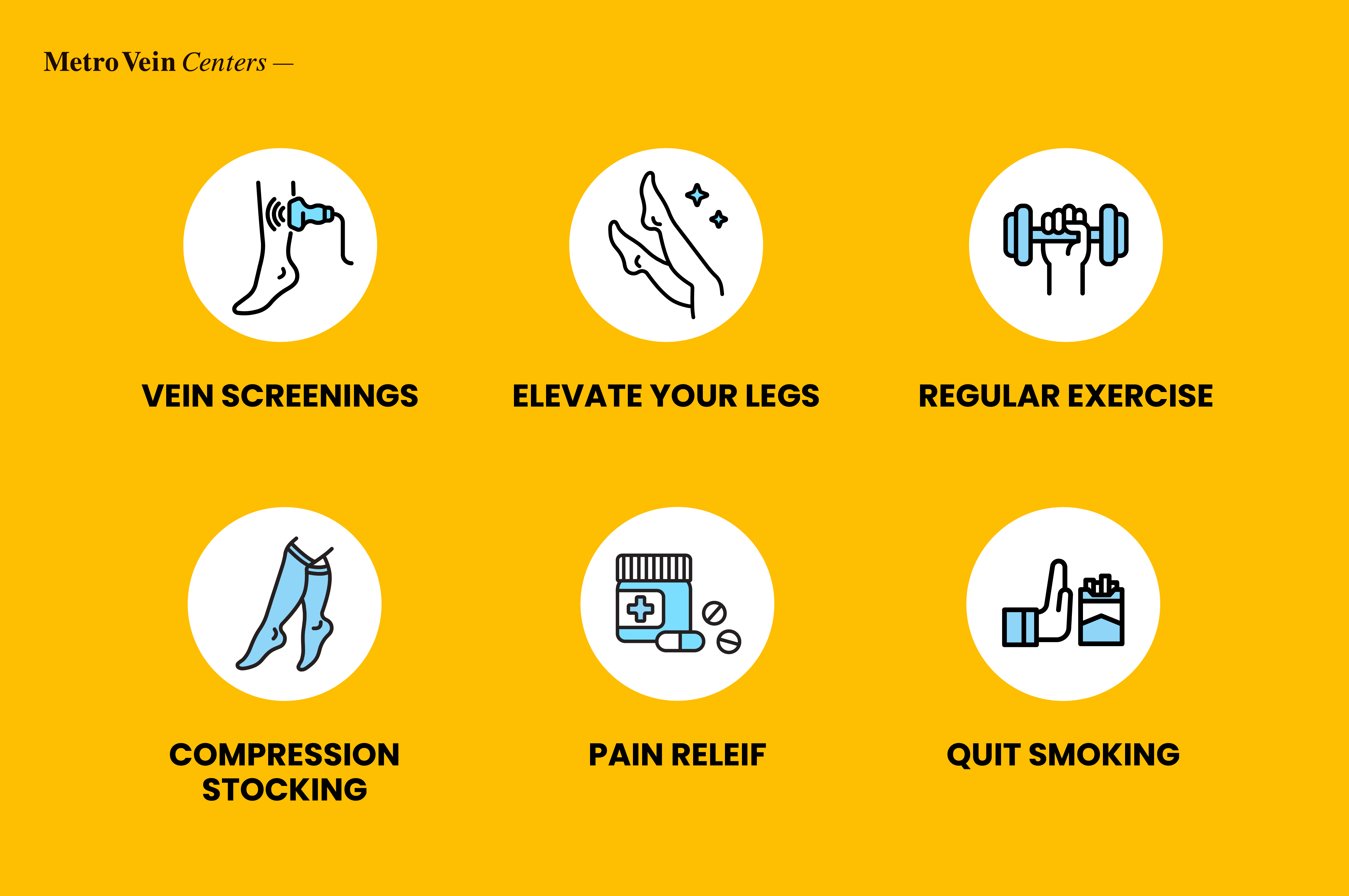
- Attend regular vein screenings to monitor its progress.
- Elevate your legs to ensure healthy blood flow to the heart.
- Get regular exercise to improve your mental well-being and blood flow.
- Wearing a compression stocking during long periods of immobility will reduce the risk of blood clotting.
- Take over-the-counter pain relief to manage pain and minor swelling.
- Enroll in a smoking cessation program to help you quit.
If you notice a sudden change in the affected area, such as excess swelling or intense pain, seek medical assistance immediately. Schedule a free comprehensive vein health evaluation with Metro Vein Centers to evaluate your risk for phlebitis.
Frequently Asked Questions:
Can phlebitis resolve on its own without treatment?
Yes, some cases of superficial phlebitis resolve without treatment.
How long does it typically take for phlebitis symptoms to improve?
Superficial phlebitis can improve within a few weeks with self-care techniques and compression therapy or medications.
Are there any natural remedies that can help with phlebitis symptoms?
Some natural remedies are touted to help with phlebitis symptoms, such as warm compresses and leg elevation. However, several studies have outlined turmeric, ginger, and garlic as natural blood thinners that can reduce the risk of blood clots.
Can air travel increase the risk of developing phlebitis?
Traveling for long periods can increase the risk of developing deep vein thrombosis. Wearing a compression stocking during travel can reduce this risk.
Is phlebitis more common in certain age groups or demographics?
Women are at a higher risk for developing phlebitis, as are people under 60.
Dr. Philip LoPresti
Meet Dr. Philip LoPresti DO, DABVLM, FACS, a board-certified vein specialist and surgeon with over 20 years of experience. Schedule an appointment with him in Queens, NY today.
Meet Dr. Philip LoPresti
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.






