Vein disease affects more than just your legs; it impacts your entire cardiovascular system and puts you at risk of serious health complications. The good news is, in most cases, vein disease is treatable using non-surgical approaches and prescription medications.
Some effective medications for vein disease include those that help thin the blood, reduce inflammation, and dissolve blood clots.
Common Vein Diseases
Veins draw deoxygenated blood from tissues and organs throughout the body and drain it into the heart for oxygenation. Therefore, to maintain a healthy heart, you need healthy veins. Unfortunately, injuries, genetic and lifestyle factors can cause vein damage and diseases that impede or slow this blood flow.
Some common vein disorders include:
- Varicose veins: Large bulging veins that are dark in color and visible through the skin.
- Deep vein thrombosis: A blood clot located in a deep vein, usually near the calf.
- Chronic venous insufficiency: Damaged veins that struggle to transport blood to the heart due to malfunctioning valves, which cause blood to pool.
The Role of Medications in Vein Disease Treatment
In certain instances, lifestyle changes alone may be sufficient to treat vein disease. Some vein disorders may require medications to alleviate symptoms, prevent complications, and improve vein health.
These medications can help thin the blood, break down blood clots, and enhance vein tone. For individuals with conditions that may impact the veins, such as high blood pressure and high cholesterol, medications to lower blood pressure and prevent plaque buildup may also become necessary.
Anticoagulants (Blood Thinners)
Anticoagulants thin the blood, helping to lower the risk of clot formation from blood clotting disorders, and treat clots when they form such as deep vein thrombosis and pulmonary embolism. Two of the most commonly prescribed anticoagulants include heparin and warfarin.
- Heparin: Prevents the formation of clots by interacting with antithrombin III, a natural inhibitor. It is administered subcutaneously or intravenously for an immediate effect.
- Warfarin: Prescribed for the long-term prevention of blood clots, especially in high-risk patients. Unlike heparin, it is administered orally, so its effects are delayed.
Thrombolytics (Clot-Dissolving Medications)
Blood thinners are used to prevent and treat blood clots, but in severe cases, thrombolytics are prescribed to dissolve these clots. Thrombolytics work by breaking down fibrin, a key component of blood clots, leading to their immediate dissolution. Conditions that may require thrombolytics include acute ischemic stroke, massive pulmonary embolism, and deep vein thrombosis.
Phlebotonics (Venotonic Agents)
Phlebotonics, also known as venotonic agents, are a specific class of medications used to alleviate symptoms of chronic venous insufficiency. They improve blood flow and venous tone by reducing inflammation.
Examples of commonly used phlebotonics include:
- Diosmin
- Hesperidin
- Gotu Kola
- Horse chestnut extract
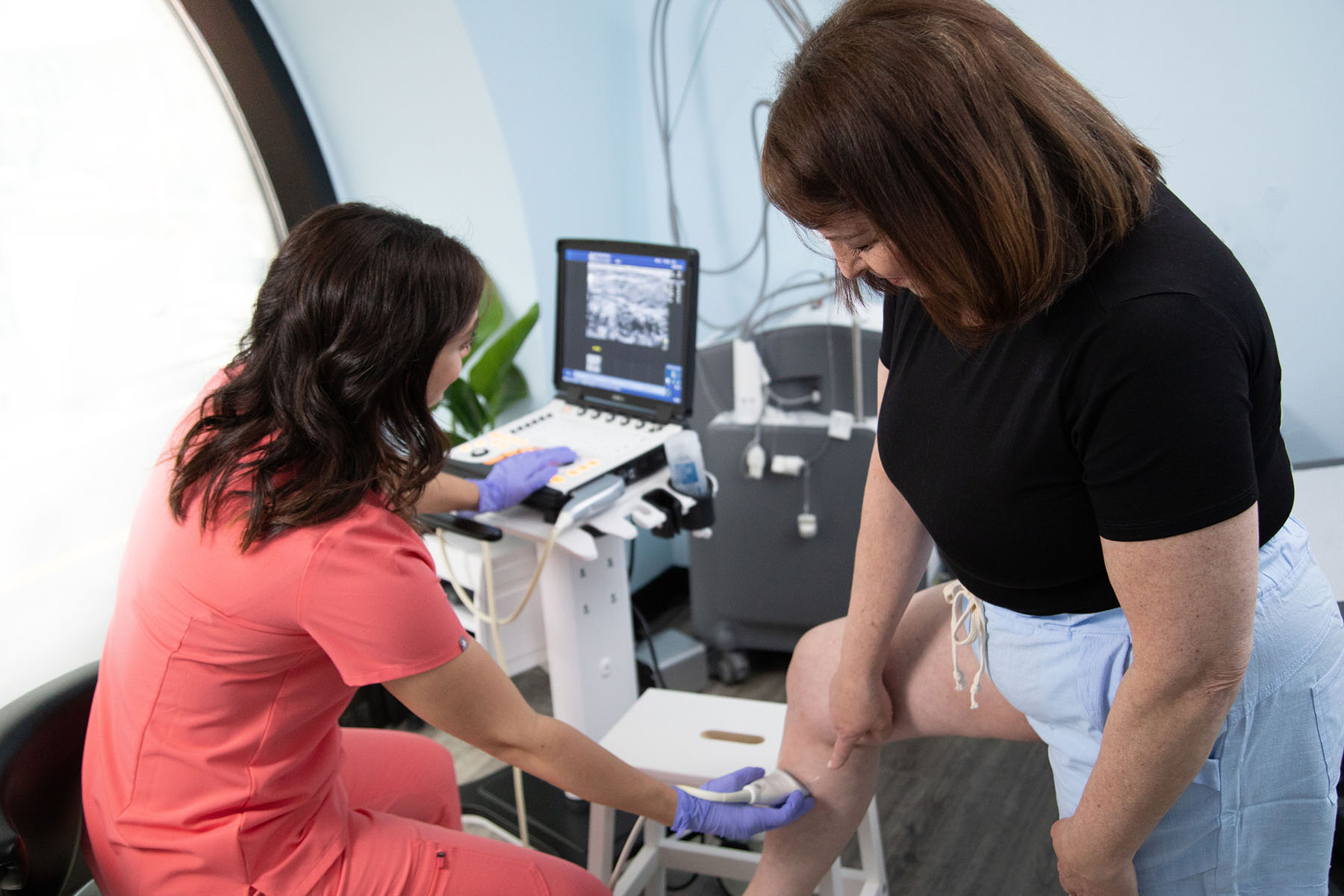
Using Sclerotherapy to Address Vein Disease
Sclerotherapy is a minimally invasive treatment used to dissolve varicose and spider veins. During this procedure, the surgeon injects sclerosant into the affected vein, which causes it to collapse and fade over time. This treatment also alleviates symptoms associated with varicose and spider veins, such as leg pain and swelling.
The Role of Compression Therapy in Treating Vein Disease
In conjunction with medications that treat varicose veins and ulcers, compression socks also play a role in reducing symptoms, helping to prevent vein damage, and reducing the risk of blood clots and deep vein thrombosis.
Compression socks come in different pressure levels and lengths and encourage muscle contraction and improve blood flow.
The Importance of Lifestyle Modifications
In addition to medication options for vein disease, there are lifestyle modifications that can also reduce the risk of worsening conditions or complications. These modifications may improve the efficacy of vein disease medications by relieving pressure on the veins and keeping them unobstructed.
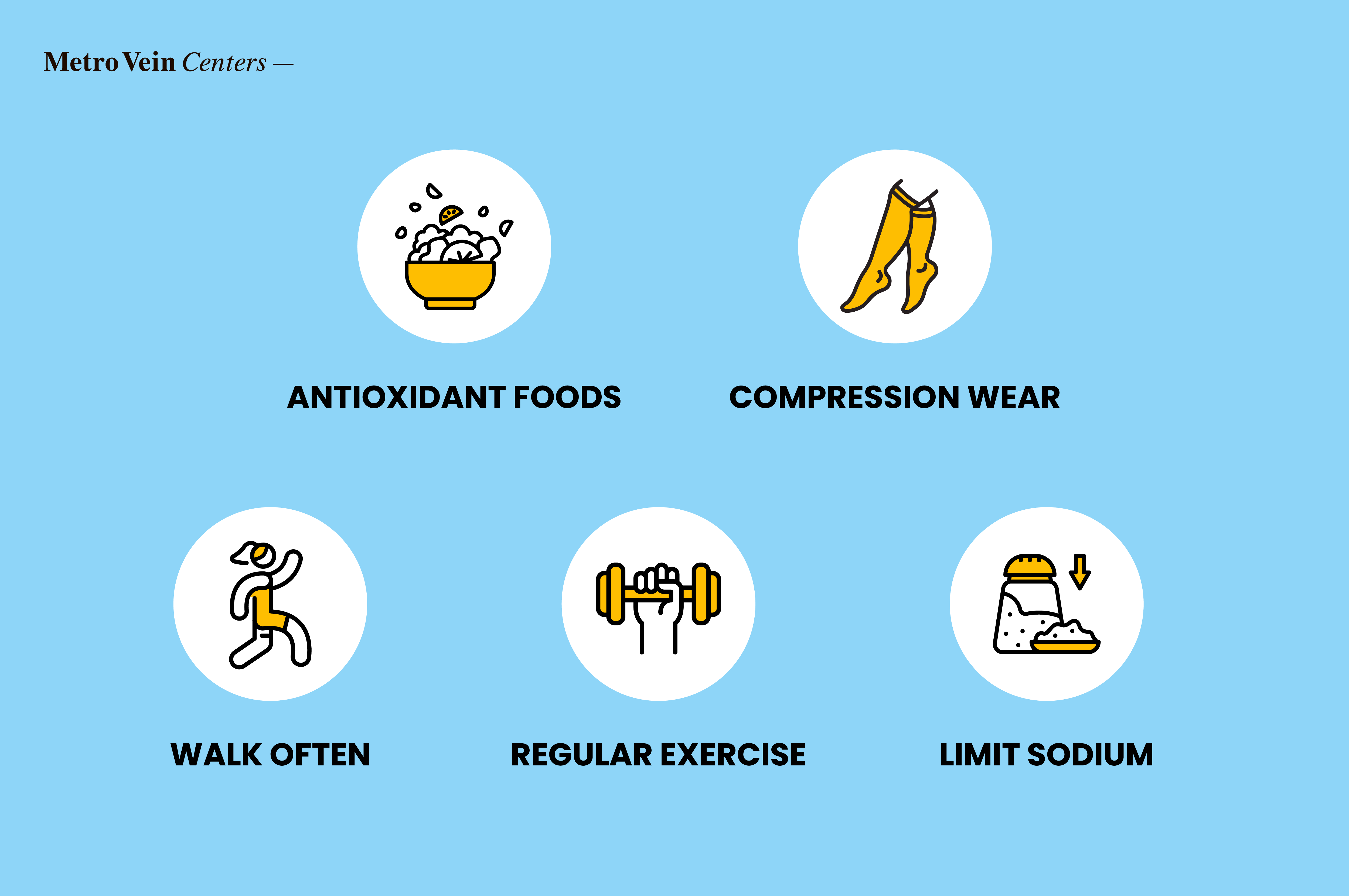
Your doctor may recommend the following lifestyle modifications to improve your vein health:
- Eat vein-healthy foods that are high in antioxidants to reduce inflammation in the veins.
- Wear compression stockings when traveling long distances.
- Walk in regular intervals to relieve venous pressure.
- Exercise regularly to help your blood flow easily.
- Reduce dietary sodium to reduce your blood pressure.
These lifestyle modifications not only improve your vein health, but your heart health as well.
Consulting a Healthcare Provider
Although medication combined with lifestyle modifications are commonly recommended for treating vein disease, you may require a different protocol based on your individual needs. For this reason, it's best to seek the advice of a vein specialist. They can help identify your specific risk factors and provide a personalized treatment plan.
Conclusion
There are several commonly-prescribed medications which have proven to be effective in treating vein disorders, including anticoagulants, thrombolytics, and phlebotonics.
To effectively manage vein disease, a vein specialist will create a personalized treatment plan tailored to your condition and unique needs. While medications such as anticoagulants, thrombolytics, and phlebotonics can help treat and, in some cases, reverse the condition, making proactive lifestyle changes is just as important to prevent vein disease from worsening or recurring.
Experiencing symptoms of vein disease? Contact our vein specialists today for a free consultation to discuss the best treatment and medication options for your condition.
Dr. Philip LoPresti
Meet Dr. Philip LoPresti DO, DABVLM, FACS, a board-certified vein specialist and surgeon with over 20 years of experience. Schedule an appointment with him in Queens, NY today.
Meet Dr. Philip LoPresti
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.