Although an incredibly common condition that affects 1 in 3 adults, vein disease is rarely discussed beyond doctors' offices. Rampant misinformation, fraudulent and ineffective products claiming impossible results, and descriptions of outdated surgical procedures all muddy up the internet. It's no wonder most people suffering from varicose veins don't realize the issue at hand... or, well, on leg.
What is vein disease? What are the stages of vein disease? Why is it important to recognize the progression of vein disease, and what can be done to stop vein disease before potentially life-threatening conditions develop -- such as deep vein thrombosis or venous ulcers? Keep reading: We've got you covered.

What is Vein Disease and Its Causes?
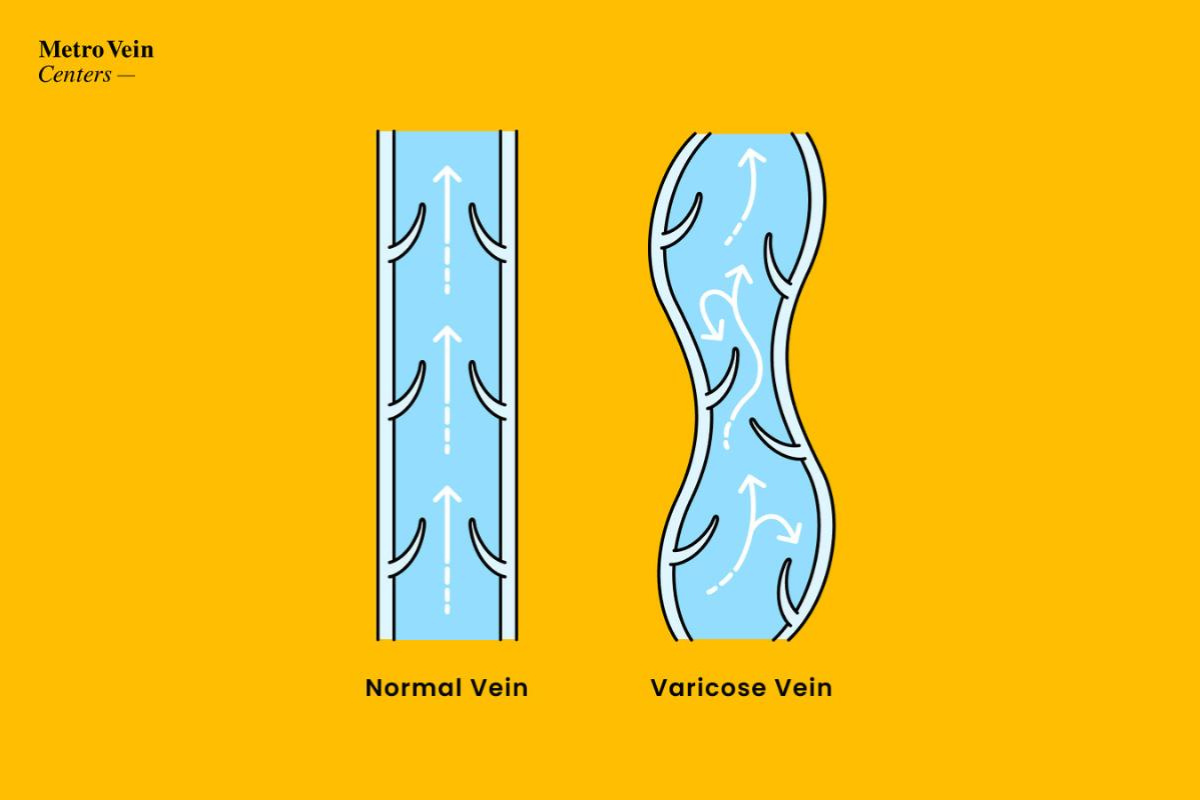
Chronic venous insufficiency (also known as "CVI" or just "vein disease") is a progressive condition that negatively affects the circulatory system. In people with vein disease, there is a structural deterioration in vein valves that allows blood to flow in the wrong direction. That creates added strain on veins, and lets blood collect instead of keep going. This can stretch and distort vein walls, leading to visibly twisted, bulging varicose veins in the legs.
The causes of vein disease vary -- and include both avoidable lifestyle choices and other unavoidable factors:
- Sex/gender (women are more likely to develop vein disease)
- Age
- Family history/genetics
- Smoking
- Pregnancy
- Use of hormonal contraceptives
- Injury (or surgery)
- Sedentary lifestyle (infrequent exercise OR jobs that require long periods of sitting or standing)
- Weight/obesity
... and more!
Now that we know some of the common causes, let's explore how vein disease develops through key stages.

Vein Disease Stages
It's important to note: Vein disease doesn't always present with visible symptoms. The bulging, twisted, cord-like varicose veins of obvious chronic venous insufficiency aren't the first flag. Typically, patients begin feeling sensations of heaviness, fatigue in the legs, and needing to elevate their feet at the end of a long day. Patients report leg swelling (also known as edema) in the feet, ankles, and calves.
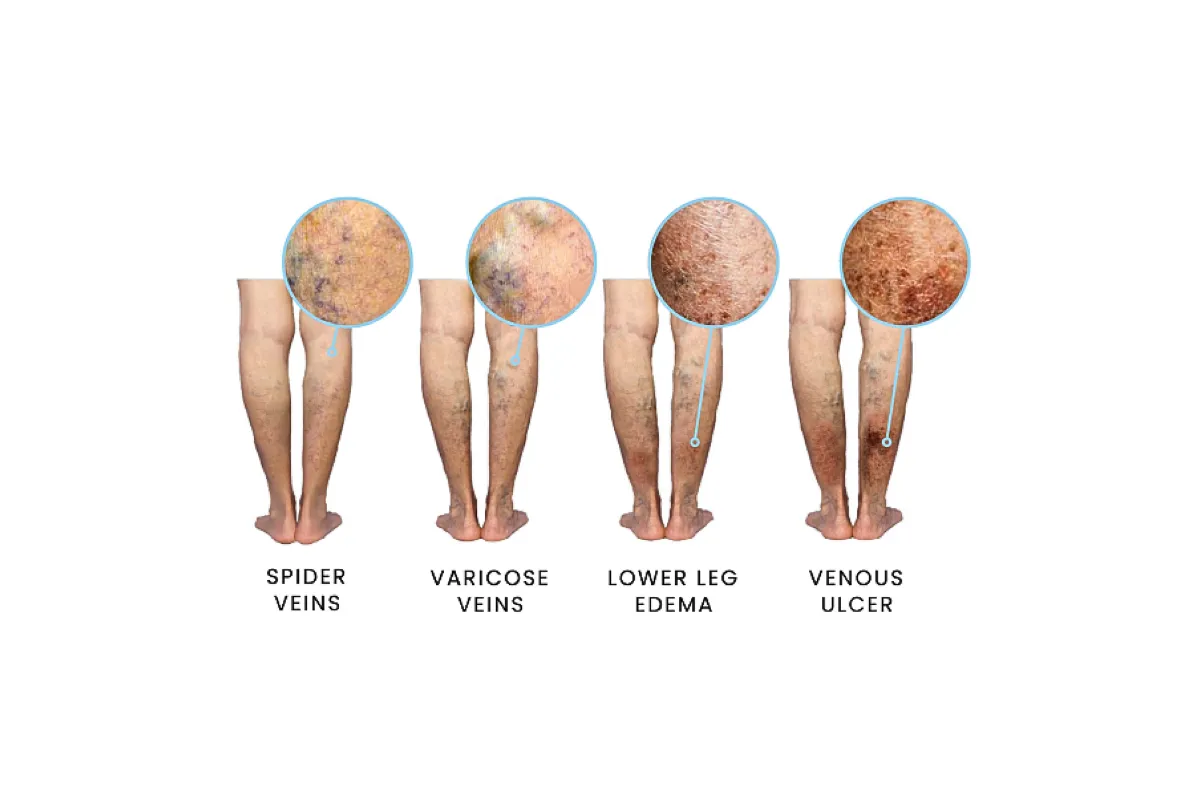
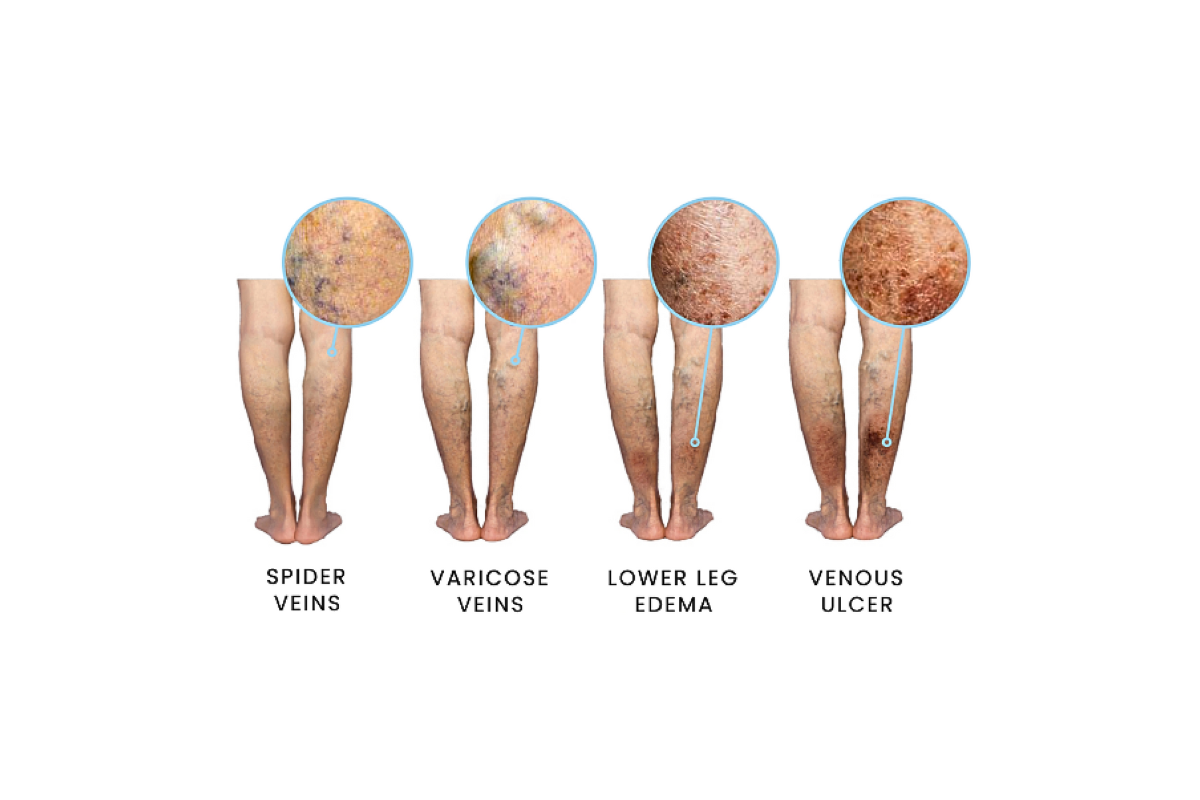
Stage 1: Visible Spider Veins
At the beginning, patients may notice signs of vein disease, with veins visible on the surface of the skin. Smaller visible veins are known as spider veins. These spider veins may be green, blue, red, or purple (depending on your skin tone). Though colorful, they are flat to the skin, and should not cause any pain.
Patients may report itching or tingling sensations as their vein health worsens. When blood begins to leak from the veins to elsewhere in your body, your immune system releases histamines to call your attention to the problem. Itching or tingling is a body's way of saying "Hey! Something's wrong, and we need help to fix it." If you see visible veins forming on your legs, or if you notice more painful or uncomfortable symptoms, it's time to talk to a vein doctor.
Stage 2: Varicose Veins Form
Varicose veins do not go away on their own.
Once they form, they can continue to develop into larger, more twisted, more visible varicose veins, and discomfort can increase. With the help of a board-certified vein specialist and FDA-approved treatments, you can get these unhealthy veins under control with approved symptoms and appearance.
Burning sensations, aching legs, and loss of mobility become more of a concern as veins are distorted by pressure from pooling blood and backward-flowing circulation. Stretched varicose veins that appear like twisting lengths of rope under the skin can cause leg cramping and restless legs. This can interfere with your sleep hygiene (how well you sleep and how restful your sleep is).
Stage 3: Leg Swelling/Edema
When it comes to swelling, we have solutions.

Our vein specialists recommend the use of compression stockings to keep swelling in check and give your circulation a much-needed boost. Experts suggest a measurement of 20-30 mmHgs of graduated compression in an over-the-knee or thigh-high stocking to help your veins keep blood flowing properly. Additionally, if you notice swelling in the legs after a day on your feet, your should elevate your legs on stacked pillows or a couch's armrest. Elevating the legs allows your veins to work with gravity rather than against it. Swelling alleviated by elevation is likely a sign that the edema you're experiencing is related to your veins.
Stage 4: Visible Skin Changes
In the late stages of vein disease, skin texture changes can occur.

Patients may see light scaling, which hardens to a sort of "elephant skin" texture. Reddening and tightening of the skin can also develop, due to long-standing swelling.
Stage 5: Healed Venous Ulcers
A venous ulcer is categorized as a wound.

Stage 6: Active (or Open) Venous Ulcers
Open ulcers, or breaks in the skin, put patients at high risk for infection and other complications. They reveal a serious impediment to the circulatory system, overall bodily health, and quality of life. It’s time to call a vein doctor.
It's important to note that vein disease, at any stage, can be treated through minimally invasive means. There are a variety of FDA-approved treatment options available provided in our vein clinics. With today's technology, no one should have to endure lengthy downtimes or even overnight hospital stays to find meaningful relief.
If this is your concern, know that you can get back to healthy, happy legs with a customized treatment plan. You do not have to live with pain.

Your Vein Evaluation
Metro Vein Centers vein specialists conduct thorough evaluations with all of our patients, discussing lifestyle, symptoms, visible changes, and new or concerning sensations. During your initial consultation, your vein specialist may decide that an ultrasound evaluation is necessary to investigate your veins from the outside in. Via ultrasound, we're able to highlight areas of concern and pinpoint malfunctioning veins painlessly and without even a needle touching your skin. Once you've shared your symptoms with your specialist, and you complete the thorough evaluation, your vein doctor will outline a care plan to address your concerns.
The number of treatments recommended, as well as the treatment type, will vary from patient to patient: No two legs are exactly the same!
We offer a variety of minimally invasive vein treatments, including:

Sclerotherapy: A sclerosing agent (a medicinal foam) is injected into the problem veins via a small needle, which causes them to gently close, allowing the body to reabsorb over time. Blood flow then is safely and gently redirected naturally through healthy veins, improving circulation. This treatment is used on both spider veins (cosmetic) and small- to medium-size varicose veins.
Radiofrequency Ablation: RFA is a varicose vein treatment option that uses pulsating radiofrequency energy to improve symptoms of vein disease. After injecting a local anesthetic, the vein specialist inserts a tiny tube into unhealthy veins. Once the radiofrequency starts pulsating and emitting heat, the vein will close and circulation will improve through healthier veins.

Endovenous Laser Ablation: EVLA uses optic fiber and laser technology. Under ultrasound guidance, the vein doctor inserts a tiny fiber into an unhealthy vein, then uses a small laser beam to heat the problem area until the valve and vein close. This promotes healthier blood flow right away.
Microphlebectomy: This treatment is a small, 2-3mm incision to permanently remove problem areas in larger, twisted veins. Instead of treating veins inside the leg, a microphlebectomy removes the specific section of a vein entirely, so bulging veins immediately disappear, blood flow increases to healthy veins, and overall leg pain decreases.
VenaSeal: This specially formulated medical adhesive is injected into a diseased vein via a tiny catheter using ultrasound guidance. With only a single injection required, VenaSeal is easy, safe, and effective. It has been proven to have a 99% success rate after six months, and is considered one of the best options for permanent removal of symptoms associated with varicose veins.

Varithena: Like sclerotherapy, this treatment is a foam medication injection into a vein using ultrasound guidance to pinpoint the precise area of need. This foam infusion causes the varicose vein to safely and gently close. Your blood then simply redirects through your surrounding healthy veins, allowing increased circulation and symptoms to improve.
Which Treatment Is Right for My Stage of Vein Disease?
Vein disease is unique to each person's veins. Each person's treatment plan will vary depending on what stage they're currently experiencing, their lifestyle choices, and what their vein specialist recommends. For smaller veins, sclerotherapy may be administered. For larger veins, a microphlebectomy or VenaSeal treatment may be recommended. There is no assigned treatment for each stage; your vein specialist's goal is to ensure you see meaningful relief and the best possible results.
Your customized treatment plan may include recommendations for lifestyle adjustments: maintaining a healthy weight, adding low-impact exercises, curbing drinking habits (caffeine and alcohol), or even quitting smoking. They may suggest using compression stockings to aid your circulatory system, or offer wound care instructions for active venous ulcers. Trust that you can always call us to speak with your patient care team and address any concerns, symptoms, or questions after your appointment.

Preventing Vein Disease
Due to the progressive nature of vein disease, many patients proactively seek evaluations to see what options are available to prevent the onset or worsening of mild symptoms. While vein disease may not be entirely avoidable due to factors like genetics, family history, pre-existing conditions (such as pregnancy or auto-immune disease), and even gender, it's important to note that best practices can set you up for healthy living.
Staying hydrated, avoiding excessive caffeine and alcohol consumption, and choosing joint-gentle exercises over heavy lifting and intensive routines can all improve your vein health. A diverse diet of nutrients, healthy fats, and proteins helps the entire body, and wearing compression stockings while on aircrafts or at work (especially if your job requires long periods of sitting or standing) can help give your veins a hand in circulating blood up from the feet.

When to Seek Medical Attention
Vein disease and poor circulation can cause a variety of uncomfortable or even painful symptoms, from itching and tingling, aching legs, leg heaviness or fatigue, swelling/edema (swollen ankles are a common complaint!), skin discolorations, restless legs that affect sleep, cramping in the legs, and more. As vein disease progresses, symptoms often become more severe, leading to complications like deep vein thrombosis (dangerous blood clots in deep veins that may lead to pulmonary embolism if left untreated), and the formation of venous ulcers. It's best to be proactive with your vein health, and to keep an eye out for worsening symptoms.
The most important thing we'd like you to take away from this article is that you can come in for an evaluation at any time, whether you have concerns for your vein health, are actively experiencing symptoms, or have noticed visible changes in your legs.
There are a few most concerning symptoms we'd like you to keep an eye on, but especially if you notice asymmetry. Swelling in only one leg, reddening of the skin in one leg but not the other, changes in the temperature of a leg, or a deep, throbbing pain in one leg, mean you should seek a vein specialist immediately to rule out the presence of deep vein thrombosis (DVT). DVTs typically occur in later stages of vein disease, and affect deep veins. Blood clots in deep veins can break away from vein walls and travel to the lungs, leading to pulmonary embolism, which can be fatal.
If you have the symptoms described above, we recommend seeking emergency care as soon as possible. If we locate a DVT in our clinic during an ultrasound evaluation, our vein specialists may put you on an anticoagulant medication or assist in getting you to emergency care.
Get Answers, Get Treatment, Get Your Legs Back
Vein disease is very common, and treatments have come a long way since the days of our grandparents. Safe, gentle, and effective options are only a phone call away! Our team of board-certified vein specialists offer vein evaluations in all of our New York, New Jersey, Connecticut, Michigan, Texas, Arizona, and Pennsylvania vein clinics. We offer minimally invasive and 100% non-invasive vein treatments for varicose veins, spider veins, and other painful or uncomfortable symptoms of vein disease. Our team is happy to answer any inquiries about treatment options, scheduling, or insurance coverage -- in fact, we accept over 200 insurance plans in our clinics! Our state-of-the-art vein treatments can be performed in under 30 minutes, in our accredited vein clinics, by our certified vein doctors. Give us a call at 866-353-5558 to schedule your vein evaluation and get started on the journey to healthy, happy legs. Whether you have questions, early symptoms, or visible concerns, we're here to help!
See our Before & After gallery, patient reviews, and patient testimonials!

"My results have been amazing. All the swelling and heaviness is gone and my legs are not burning after a long day. Their team is professional and competent."
- Opal, Warren
"Whether the issue at hand is merely cosmetic or debilitating pain, nothing changes the fact that someone's quality of life is on the line. Patience and communication are paramount to successful diagnoses and treatments."
- Dr. Philip LoPresti
Dr. Philip LoPresti
Meet Dr. Philip LoPresti DO, DABVLM, FACS, a board-certified vein specialist and surgeon with over 20 years of experience. Schedule an appointment with him in Queens, NY today.
Meet Dr. Philip LoPresti
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.