Varicose veins are often perceived as a condition that predominantly affects women, but an estimated 11 million men also suffer from this health issue. While women typically receive information from family and friends about what to look for, men are often less willing to discuss the condition or seek treatment. This reluctance can lead to worsening symptoms and serious complications over time.
In this guide, you'll learn how varicose veins affect men, the signs to watch for, the available treatment options, and the critical importance of early screening. By understanding this condition, men can take proactive steps to address it before it worsens.
Prevalence of Varicose Veins in Men
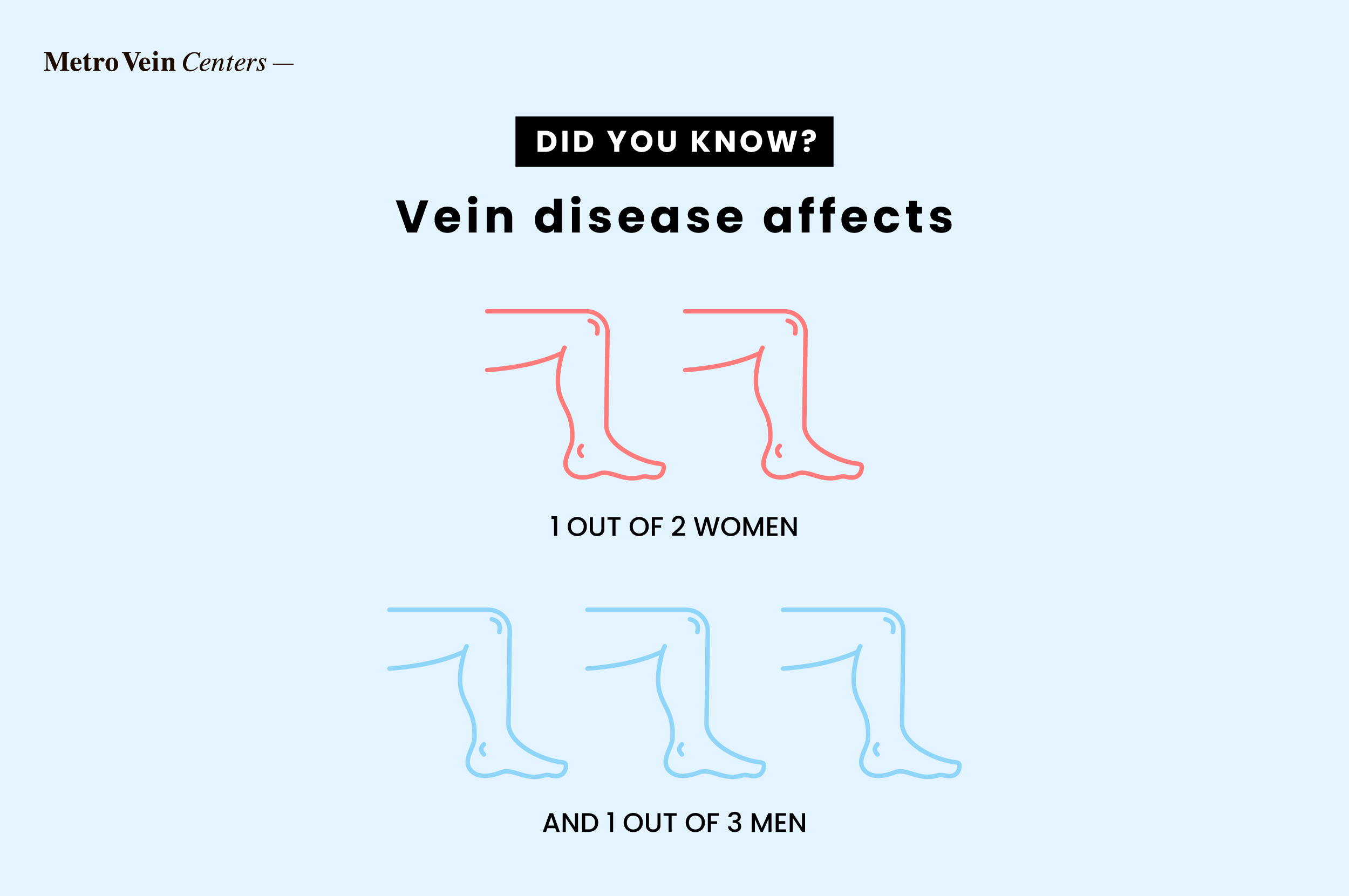
Varicose veins are often mistakenly believed to be a cosmetic issue that only affects women. In reality, while they are more prevalent in women--affecting approximately 20-25% of them--men can also develop this condition. It's important to recognize that varicose veins can affect anyone, regardless of gender.
Statistics on Occurrence in Male Population
A recent study published by Sage Open Medicine found that approximately 10-15% of men in Western and developed nations develop varicose veins. While this statistic demonstrates a lower instance of varicose veins in men than women, it does point to a growing trend of varicose veins in the male population.
Debunking the "Women's Issue" Myth
The American Heart Association (AHA) identifies being female as a significant risk factor for developing varicose veins. This risk factor often leads to the misconception that only women can have this condition. While women are indeed at higher risk due to hormonal influences from progesterone and estrogen--varicose veins can also affect men. Around 11 million men between the ages of 40 and 80 struggle with this condition, highlighting that a variety of risk factors impact both genders.

Causes and Risk Factors Specific to Men
Varicose veins develop when the valves in the veins weaken or get damaged, which disrupts normal blood flow. This disruption leads to blood pooling in the veins, causing them to stretch and have a twisted appearance, often seen as the squiggly or web-like patterns of varicose and spider veins.
While genetics can increase the risk of developing varicose veins, other factors, such as smoking and sitting for extended periods, can also contribute to their formation.
Genetic Predisposition
Like other hereditary conditions, men who have close family members with varicose veins may also develop them. Additionally, a small study published by the American Heart Association found that individuals with certain genetic mutations are also at a significantly higher risk.
Occupational Risks
Another common risk for developing varicose veins is sitting or standing for extended periods. According to Johns Hopkins Medicine, standing or sitting for a prolonged period can cause blood to pool in the veins, leading to increased pressure within the vein that distorts its appearance.
Lifestyle Factors Affecting Vein Health
A number of lifestyle factors can affect vein health, leading to conditions like venous insufficiency (a form of chronic venous disease), varicose, and spider veins.
This includes:
- Smoking
- Obesity
- Hormone use
- Inactivity
- Wearing tight clothing

Recognizing Varicose Veins in Men
Varicose veins develop over many years, so you may not notice them initially. When you do, their appearance can be quite alarming. You will likely see them on or near your calf muscle, though they can appear anywhere on the leg or the body. If you spot a varicose vein, it is important to seek treatment options right away to prevent complications.
Visible Signs and Symptoms
A varicose vein will stand out from a typical vein's appearance. While other veins remain hidden just beneath the surface of your skin, varicose veins bulge out with a squiggly, bluish-purple appearance. These veins may itch or cause mild pain.
Other signs and symptoms include:
- Leg pain
- Skin discoloration in the affected area
- Swelling in the area
- Nighttime leg cramps
When to Seek Emergency Medical Attention
If you feel a hard lump, notice the area is warm to the touch, swollen, or highly uncomfortable, seek medical attention immediately.
These symptoms can indicate a blood clot.

Diagnosis and Assessment for Male Patients
The most common approach to diagnosing a varicose vein begins with a physical examination. During this exam, the doctor will assess visible signs of varicose veins and inquire about any symptoms you may be experiencing.
To gain a deeper understanding, they may also perform diagnostic tests such as vein mapping that utilizes a venous duplex ultrasound (DUS) for a more detailed look at the veins.
Vein Mapping and Ultrasound Procedures
Vein mapping--is a diagnostic procedure that uses a duplex ultrasound (DUS) to view and take pictures of the veins in your legs. Ultrasound technicians use this technique to 'map' the veins in your legs and look for blockages and damage. They might also use a duplex ultrasound during a treatment procedure to guide them to the designated areas needing treatment.

The Importance of Early Detection
Early detection of varicose veins prevents them from worsening and causing complications such as blood clots or ulcers, which can be life-threatening. They are also much easier to treat in the earlier stages. The longer you wait to have your varicose veins treated, the more invasive the treatments may become.
Treatment Options Tailored for Men
Treatment options for varicose veins in men begin with non-invasive conservative approaches and expand to include laser treatments and surgical interventions like vein stripping. The most common treatments are compression stockings, Sclerotherapy, and Radiofrequency Ablation (RFA).
Conservative Approaches (Compression Stockings)
Compression stockings can help manage symptoms associated with varicose veins. They work by applying pressure at the ankle and gradually releasing the pressure toward the opening of the stocking. This stimulates circulation, moving blood from the leg to the upper body. They also reduce leg swelling, which can contribute to worsening varicose veins and blood clots.
Compression stockings are divided into classes, each denoting a different grade of pressure. Class 1 or low-pressure compression stockings treat mild swelling and discomfort in the leg. Class 2 or medium-pressure compression stockings treat varicose veins. Class 3 or high-pressure compression stockings treat serious conditions such as blood clots and severe venous conditions.
Minimally Invasive Procedures (Sclerotherapy, RFA)
When compression stockings aren't enough to treat varicose veins, a procedure is the next step. Luckily, there are several minimally invasive procedures that vascular surgeons use to remove and treat varicose veins.
Popular choices include:
- Sclerotherapy: During a sclerotherapy treatment, a chemical solution is injected into the vein, causing it to close. The body then reabsorbs the vein and redirects blood flow to nearby veins.
- RFA: Radiofrequency Ablation, is a varicose vein treatment option that uses pulsating radiofrequency energy to improve symptoms of vein disease.
Recovery and Downtime Considerations
Sclerotherapy and RFA have little to no downtime, and you can return to your regular activities on the same day in most cases. However, you should avoid strenuous exercise or moving heavy objects for a few weeks after either procedure. You should also avoid direct sunlight as the scar can darken (hyperpigmentation). Your physician might also direct you to wear compression stockings for a few weeks after having the procedure.

Prevention Strategies for Men
Some men develop varicose veins because of a genetic predisposition, but in some cases, they are preventable. The best methods to prevent varicose veins are to maintain a healthy weight, stay active, and avoid unhealthy lifestyle choices such as smoking.
Exercise Recommendations
According to the Centers for Disease Control and Prevention (CDC), adults, regardless of gender, need 150 minutes of exercise or 75 minutes of vigorous, intense activity each week. They also recommend at least two days of strength training per week. Following these guidelines can help you to maintain a healthy weight and improve your circulation and heart health.
Dietary Considerations
Foods contributing to high blood pressure, high cholesterol, and obesity should be avoided or reduced to decrease your risk of developing varicose veins.
This includes foods high in saturated or trans fats, cholesterol, sodium, and sugar.
Examples are:
- Hotdogs
- Pie
- Full-fat cheese
- Pizza
- White bread
- French fries
- Frosted cereals
Workplace Modifications
If you work a sedentary job, there are several modifications you can make to reduce your risk of varicose veins.
They include:
- Taking a walk every few hours
- Walking during breaks
- Bringing a healthy lunch to avoid vending machine foods
- Staying hydrated throughout the day
- Using a standup desk with an under-desk treadmill
- Using an under-desk stepper or elliptical to keep your legs moving
- Flexing your feet back and forth regularly to improve blood flow to your legs

Living with Varicose Veins: A Man's Perspective
Men feel just as uncomfortable about having varicose veins as women do. The condition can distort the way the legs look, causing self-consciousness and even throbbing pain throughout the day, affecting your quality of life. Some men even have difficulty playing sports or working out until they are treated.
Impact on Daily Activities and Athletic Performance
Varicose veins can significantly impact an athlete's overall performance, leading to reduced speed or missed games due to severe pain or swelling. This discomfort is often the result of increased pressure on the varicose veins, which can occur from lifting heavy weights, jumping, or running. Some individuals even experience pain while cycling.
Addressing Aesthetic Concerns
Dark or bulging varicose veins can look unsightly, which is why some men avoid showing their legs. The good news is that they are treatable. If caught early enough, the treatments are minimally invasive and leave little to no scarring.
We're Here to Help
At Metro Vein Centers, our board-certified vein specialists are experts at detecting and treating varicose and spider veins with non-invasive and minimally invasive procedures. Many of our treatments are performed in under 30 minutes, with little to no downtime. Should you require treatment, we accept over 200 insurance plans.
If you suspect a varicose vein, visit one of our New York, New Jersey, Pennsylvania, Connecticut, Michigan, Texas, or Arizona clinics, where we offer free vein screenings. To book, give us a call at 866-353-5558 today.
FAQs:
Can weightlifting cause varicose veins in men?
While weightlifting doesn't cause varicose veins, in some cases, strenuous exercise, especially if it involves heavy lifting, might exacerbate the condition.
Are varicose veins in men more common in certain professions?
Yes. Men working in any sedentary capacity, including graphic designers, delivery drivers, and customer service representatives, are at a greater risk of developing varicose veins.
How does testosterone affect varicose vein development in men?
Testosterone does not cause varicose veins, though low levels can lead to estrogen dominance, placing older men at risk of developing them.
What's the typical recovery time for men after varicose vein treatment?
Depending on the treatment, a full recovery can take one to four weeks.
Can varicose veins in men lead to more serious health issues if left untreated?
Yes, if left untreated, varicose veins can lead to blood clots, bleeding through the skin, ulcers, and edema.
Book a consultation to discuss your personalized treatment plan.
Dr. Philip LoPresti
Meet Dr. Philip LoPresti DO, DABVLM, FACS, a board-certified vein specialist and surgeon with over 20 years of experience. Schedule an appointment with him in Queens, NY today.
Meet Dr. Philip LoPresti
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.