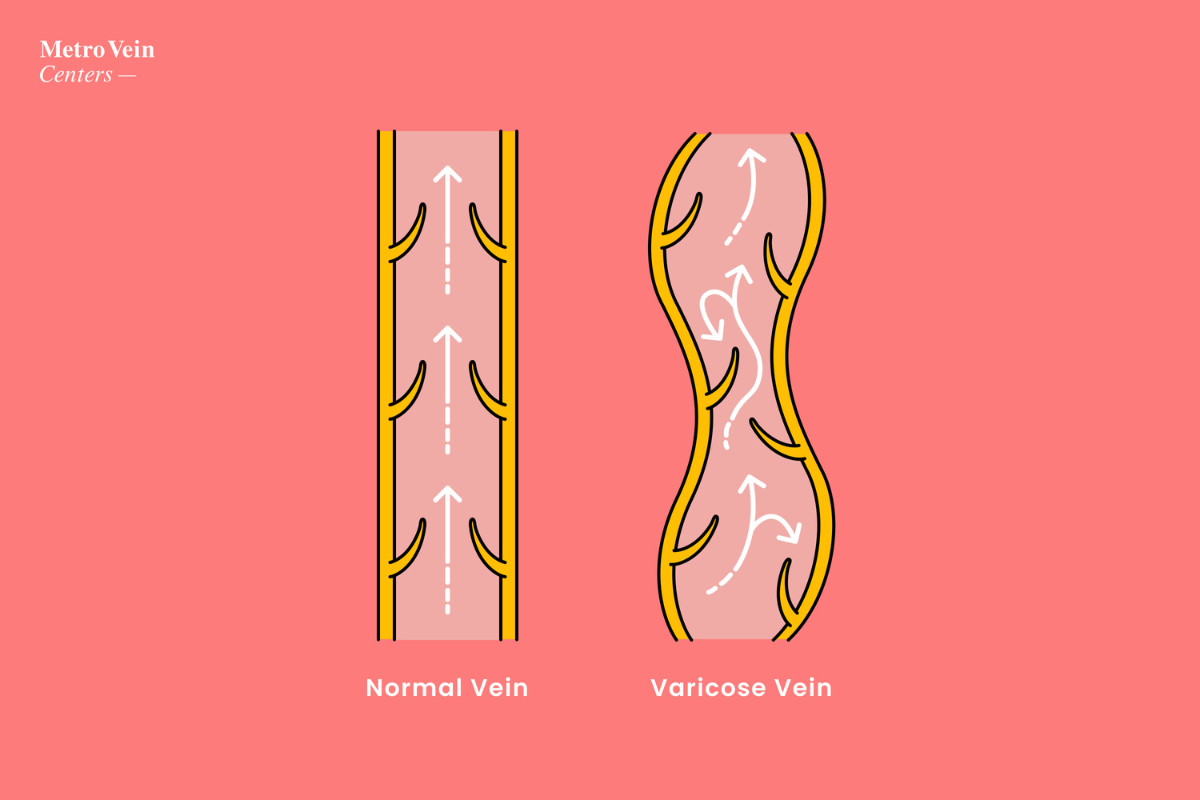
Vein disease is a progressive condition that 1 in 3 adults experience at some point in their lives.
Regardless of how healthy someone is overall, genetic predispositions and lifestyle choices can affect the onset and progression of chronic venous insufficiency, which includes varicose veins and other uncomfortable symptoms.
Absolute prevention is not scientifically possible because of factors like autoimmune disease, sex/gender, pregnancy, and age, which are entirely outside our control. However, there certainly are controllable factors which can accelerate or worsen vein disease.
Some genetic factors and lifestyle choices that increase your risk of developing varicose veins include:
1. Sex/Gender
Women are more likely than men to develop vein disease.
2. Age
People over the age of 45, and especially those over 60, experience symptoms of vein disease at a higher scale than people in their 30s -- though it is not impossible to experience vein disease before the age of 45.
3. Genetics and Inherited Disease
If your family members have signs or symptoms of vein disease, you are significantly more likely to develop varicose veins. Additionally, certain conditions genetically predispose you to vein disease, such as diabetes and celiac disease. These can all affect your circulation and increase your chances of developing varicose veins.
4. Pregnancy
A higher volume of blood in the body plus the excess strain of gravity on your lower legs due to a growing belly puts pressure on your veins and can lead to the development of varicose veins during pregnancy and postpartum.
5. Smoking
Smoking causes vasoconstriction, or a tightening/narrowing of the veins. When veins are constricted, it is difficult for blood to move through uninhibited. Bulging veins and broken or leaky vein valves (which control blood's one-way route) can be a result of constricted veins.
Solution: Limiting tobacco usage, or quitting altogether (which is easier said than done, we know), will reduce constriction in your veins and allow blood to flow normally through healthy veins.
6. Excessive Caffeine
Caffeine can temporarily constrict blood vessels and mildly elevate blood pressure. While this effect is generally short-term, prolonged high caffeine consumption may strain vein valves, especially in those already at risk for vein problems.
Before anyone says it, we're not asking you to give up your daily cup of joe. Excessive caffeine (we're talking 3+ cups per day) acts as another vasoconstrictor, which inhibits the ease of blood flow.
Solution: Consume caffeine in moderation, keeping your daily intake below 400 milligrams. Additionally, drink plenty of water to stay hydrated, which can help offset caffeine intake and keep your blood flowing strong.
7. Frequent Alcohol Consumption
Alcohol is a vasodilator, the opposite of a vasoconstrictor. Vasodilation abnormally expands the veins and allows more blood to flow. If you consume alcohol on a daily basis, or consume large amounts of alcohol regularly, this can be too much for your veins to bear. This can lead to malfunctioning valves and blood pooling in the veins.
Solution: If you drink regularly, opting for soft drinks or mocktails more often might help curb your appetite for vasodilating alcoholic beverages.

8. Stress
We're sure you've heard "reduce your stress levels" at least once at a doctor's office. In a world that's as fast-paced as it is noisy, it can seem unattainable to find calm in your day-to-day life. However, it's important to try to reduce stress where possible; high levels of stress impact your entire body, brain to vein, and can cause vasoconstriction of your veins.
Solution: Finding time for mindfulness, reducing late nights at work, or even taking some time to breathe or do yoga more often can help reduce critical stress levels.
9. Frequent Flying
Spending long periods of time sitting in the sky (plus the pressure changes within aircraft cabins) reduces blood flow. Lack of movement for extended periods of time, which we'll discuss further in our next point, can put excess stress on the veins.
Solution: When you fly, wear medical-grade compression stockings and make sure to stretch or walk the aisles every so often to get your blood pumping again!
10. Long Periods of Sitting or Standing
Because so many of our jobs require sitting in cubicles/office environments or standing behind registers, it can be difficult to find time to stretch or rest our legs. This strain, aided with the heavy hand of gravity, can damage the stability of your veins.
Solution: Compression stockings! These garments keep light pressure on your legs, not unlike muscle movement, which can help blood to flow smoothly through your healthy veins back towards your heart. We recommend over-the-knee stockings that can be worn beneath pants or by themselves. Elevating your legs after work can also relieve some of the strain of a long day of sitting or standing. Kick up your feet!

How We Can Help
Although avoiding vein disease simply may not be in the cards for those with genetic predispositions, good lifestyle choices can help stave off symptoms and keep them milder for longer, delaying the worsening of varicose veins. Good vein health, such as staying hydrated, pursuing light or low-impact exercise, eating iron-rich foods, and more will keep your blood flowing strong. Elevating your feet during extended periods of sitting, or pausing to stretch during leisure time, can also benefit your vein health.
These choices can improve your vein health and lessen the severity of your symptoms, but the best course of action when/if you notice persistent symptoms of vein disease -- such as visible varicose veins, swelling, restless legs (especially if they are impacting your ability to sleep at night), aching, itching, etc. -- is to proactively seek vein treatment. Vein disease is progressive, which means it will worsen over time if left untreated. Vein disease does not go away on its own and can lead to more severe symptoms such as venous ulcers and wounds on your legs if not addressed. The good news is that vein disease is easily treatable (and results are permanent) with modern advances in vein treatment.

Metro Vein Centers offers free vein evaluations in all of our New York, New Jersey, Connecticut, Michigan, and Texas vein clinics, and our board-certified teams of vein specialists provide FDA-approved, minimally invasive vein treatments for both varicose veins and spider veins. The first step toward improving your vein health may be cutting out that fourth cup of coffee, or wearing compression socks to your day job. But know that true, lasting relief is only a phone call away.
We accept over 200 insurance plans for our varicose vein treatments, and we're happy to speak with your insurance company directly to ensure you get the maximum coverage possible. We'll work with you to address your specific concerns and symptoms, and we'll take your lifestyle into account when we customize your vein treatment plan. Vein disease may not be avoidable for us all, but it is 100% treatable without overnight or extended hospital stays. All of our state-of-the-art vein treatments are performed in less than 40 minutes, in our clinics, by our nationally accredited vein doctors.
Give us a call, and get a leg up on vein disease. We look forward to seeing you!
Dr. Philip LoPresti
Meet Dr. Philip LoPresti DO, DABVLM, FACS, a board-certified vein specialist and surgeon with over 20 years of experience. Schedule an appointment with him in Queens, NY today.
Meet Dr. Philip LoPresti
Trusted insight from the nationally accredited, board-certified vein doctors at Metro Vein Centers.